Difference between revisions of "Disease Detectives"
m |
|||
| Line 164: | Line 164: | ||
[https://www.cdc.gov/ophss/csels/dsepd/ss1978/lesson5/section1.html Public Health Surveillance - CDC] | [https://www.cdc.gov/ophss/csels/dsepd/ss1978/lesson5/section1.html Public Health Surveillance - CDC] | ||
| − | ==How to prove x caused y, or | + | ==How to prove x caused y, or Cause== |
==Types of Carriers/Vectors== | ==Types of Carriers/Vectors== | ||
Revision as of 20:31, 21 March 2020
Template:EventLinksBox Disease Detectives is an event in Division B and Division C that focuses on epidemiology, the study of diseases and how they spread.
Focus Topics
Disease Detectives rotates between topics every two years. Typically the topic has a minor impact on the content of the event, usually only affecting the specific types of diseases used in problems. However, now Disease Detective includes disease from all topics. Therefore, there is no given one.
| Year | Topic |
|---|---|
| 2018 | Food Borne Illness |
| 2017 | |
| 2016 | Population Growth |
| 2015 | |
| 2014 | Environmental Quality |
| 2013 | |
| 2012 | Food Borne Illness |
| 2011 | |
| 2010 | Population Growth |
| 2009 | |
| 2008 | Environmental Quality |
| 2007 |
Event Format
The Foodborne Illness focus covers areas that include:
- Historical foodborne illness outbreaks
- Characteristics of different foodborne illnesses (salmonella, botulism, etc.)
- Safe cooking temperature for different foods
- Prevention techniques for stopping foodborne illness transmission
- Food preparation steps and safety
- Pulsenet and other national surveillance techniques for foodborne illnesses
The Population Growth focus covers areas that include:
- Water Quality, Water Pollution, Water Demands
- Sanitation Needs
- Growth of Slums and Household Environment
- Environmental Degradation
- Air Pollution
- Infectious Disease Outbreaks
- Rapid Spread of Disease via Public Transportation and Air Travel
- Food Quality and Food Contamination
- Lack of food in poor nations vs. unhealthy fast food and drinks in technological societies
- Availability of health care for the poor and the aged
- People moving into uninhabited areas
- New pathogens, such as Lyme disease and Ebola
The Basics
Epidemiology
Epidemiology is the study of distribution and determinants of health-related states in specified populations, and the application of this to control health problems. There are four basic reasons for why disease detectives study and research outbreaks and epidemics. These reasons are: Control and Prevention, Research Opportunities, Training, and Legal Concerns.
Two Basic Types of Epidemiology
- Classical Epidemiology - population oriented, studies community origins of health problems related to nutrition, environment, human behavior, and the psychological, social, and spiritual state of a population. The event is more aimed towards this type of epidemiology.
- Clinical Epidemiology - studies patients in health care settings in order to improve the diagnosis and treatment of various diseases and the prognosis for patients already affected by a disease. These can be further divided into:
- Infectious Disease Epidemiology - heavily dependent on laboratory support
- Chronic Disease Epidemiology - dependent on complex sampling and statistical methods
There are all sorts of classification systems for epi and the above certainly are examples. One could add research epi vs applied epi to the above list. However probably the most fundamental and common system is Descriptive epi (e.g. person, place and time) vs Analytic epi (hypothesis testing - study design).
Basic Epidemiology Terms
- Cluster - An aggregation of cases over a particular period closely grouped in time and space, regardless of whether the number is more than the expected number
- Endemic Disease - Present at a continuous level throughout a population/geographic area; constant presence of an agent/health condition within a given geographic area/population; refers to the usual prevalence of an agent/condition.
- Epidemic - Large numbers of people over a wide geographical area are affected.
- Etiology - Study of the cause of a disease.
- Fomite - A physical object that serves to transmit an infectious agent from person to person. An example of this is lice on a comb. The comb is the fomite and the lice are the agent that can make your hair itch.
- Iatrogenic- An illness that is caused by a medication or physician.
- Incubation Period - Time in between when a person comes into contact with a pathogen and when they first show symptoms or signs of disease.
- Index Case - First patient in an epidemiological study (also known as patient zero or primary case).
- Latent Period - Time in between when a person comes into contact with a pathogen and when they become infected.
- Morbidity - Rate of disease in a population.
- Mortality - Rate of death in a population.
- Outbreak - More cases of a particular disease than expected in a given area or among a specialized group of people over a particular period of time.
- Pandemic - An epidemic occurring over several countries or continents and affecting a large proportion of the population.
- Plague - A serious, potentially life-threatening infectious disease that is usually transmitted to humans by the bites of rodent fleas. It was one of the scourges of our early history. There are three major forms of the disease: bubonic, septicemic, and pneumonic.
- Nosocomial Disease - An infection that is acquired in a hospital.
Risk - The probability that an individual will be affected by, or die from, an illness or injury within a stated time or age span. Risk of illness is generally considered to be the same as the Incidence (see below) and the terms are used interchangeably. Age-span is not usually a consideration in this usage. Risk of death from a particular illness is expressed as the Case Fatality Rate (Number deaths due to a disease/Number with the disease) or the Cause-specific Mortality Rate (Number deaths due to a disease/Number in population). Age span is a more common consideration in this last usage.
- Surveillance - The systematic and ongoing collection, analysis, interpretation, and dissemination of health data. The purpose of public health surveillance is to gain knowledge of the patterns of disease, injury, and other health problems in a community so that we can work towards their prevention and control.
- Vector - An animal that transmits disease. For example, a mosquito is a vector for malaria.
- Zoonosis - An infectious disease that is transmissible from animals to humans.
- Symptomatic - Showing symptoms or signs of injury.
- Asymptomatic - Showing no signs or symptoms, although can be carrier of disease.
Incidence, Prevalence, and Duration
The incidence of an illness is the number of new instances of disease in a population over a given time period. It is expressed as "X cases/Y population/ Z time". The prevalence of an illness is the number of affected persons in the population at any given point in time. It is expressed as "X cases/Y population". There are two major ways in which prevalence is measured: period prevalence and point prevalence. Think of point prevalence as a snapshot of the population and its rate of a certain disease at a point in time while period prevalence tracks the prevalence over a certain duration. Note the only difference is that incidence (I) includes time while prevalence (P) does not. Time (D) reflects the duration of the illness or condition. If two conditions have the same incidence in a population, the one with the longer duration will have the greater prevalence. Importantly, [math]P = I*D[/math], so with two of the variables, it is possible to solve for the third.
Thirteen Steps to Investigating an Outbreak
Remember that this is a conceptual order, so steps have to be done simultaneously!
- Prepare for field work
- Establish the Existence of an Outbreak - Consider Severity, Potential for Spread, Public Concern, and Availability of Resources
- Verify the Diagnosis
- Construct a Working Case Definition
- Find Cases Systematically and Record Information
- Describe and Orient the Data in Terms of Person, Place, and Time - Descriptive Epidemiology
- Develop Hypotheses (Agent/Host/Environment Triad) = Chain of Transmission
- Evaluate Hypotheses - Analytical Studies (MUST Have a Control Group)
- Refine Hypotheses if Necessary
- Compare and Reconcile with Laboratory and/or Environmental Studies
- Implement Control and Prevention Measures (ASAP!)
- Initiate or Maintain Surveillance
- Communicate Findings
Ten Steps to Outbreak Investigation - Explanation of Steps
Five Step Process for Surveillance
- Identify, define, and measure the health problem of interest
- Collect and compile data about the problem (and if possible, factors that influence it)
- Analyze and interpret these data
- Provide these data and their interpretation to those responsible for controlling the health problem
- Monitor and periodically evaluate the usefulness and quality of surveillance to improve it for future use. Note that surveillance of a problem does not include actions to control the problem
Public Health Surveillance - CDC
How to prove x caused y, or Cause
Types of Carriers/Vectors
- Convalescent-Humans are also capable of spreading disease following a period of illness, typically thinking themselves cured of the disease.
- Incubatory-When an individual transmits pathogens immediately following infection but prior to developing symptoms
- Chronic-Someone who can transmit a disease for a long period of time
- Genetic-has inherited a disease trait but shows no symptoms
- Transient/Temporary-Someone who can transmit an infectious disease for a short amount of time
Hill's Criteria for Causation
Nine criteria must be met to establish a cause-and-effect relationship. This is commonly known as Hill's Criteria for Causation:
- Strength of Association - relationship is clear and risk estimate is high
- Consistency - observation of association must be repeatable in different populations at different times
- Specificity - a single cause produces a specific effect
- Alternative Explanations - consideration of multiple hypotheses before making conclusions about whether an association is causal or not
- Temporality - cause/exposure must precede the effect/outcome
- Dose-Response Relationship - an increasing amount of exposure increases the risk
- Biological Plausibility - the association agrees with currently accepted understanding of biological and pathological processes
- Experimental Evidence - the condition can be altered, either prevented or accelerated, by an appropriate experimental process
- Coherence - the association should be compatible with existing theory and knowledge, including knowledge of past cases and epidemiological studies
Hill's Criteria for Causation Explanations and History
Epidemiological Triads
Epidemiologists use two triads. The first is the foundation for descriptive epidemiology - person, place and time. The second is described in the next section.
Chain of Transmission Triad
This is another common triad, which is an altered form of the Chain of Infection described below. It is a companion to the Epidemiological Triad. It also has three components:
- An external agent
- A vector or fomite that transmits the disease
- A susceptible host for the disease
This is used to define the major points of a disease case.
Epidemiological Study Designs
Basic Studies
- Ecological - comparisons of geographical locations
- Cross Sectional - a survey,health questionnaire, "snapshot in time"
- Case-Control - compare people with and without disease to find common exposures
- Cohort - compare people with and without exposures to see what happens to each
- Randomized Controlled Trial - human experiment
- Quasi Experiments - research similarities with traditional experimental design or RCT, but lack element of random assignment to treatment/control
Advantages and Disadvantages to Study Designs
| Study Designs | Advantages | Disadvantages |
|---|---|---|
| Trial |
|
|
| Cohort Study |
|
|
| Case-Control Study |
|
|
| Cross-Sectional Study |
|
|
2x2 Table
A table which has two columns and rows for people with or without exposure and with or without disease; shows the number of people with each characteristic.
| Disease | No Disease | |
|---|---|---|
| Exposure | a | b |
| No Exposure | c | d |
Using the 2*2 Table, we can calculate the odds ratio and relative risk. These calculations allow comparisons between the control group and the group afflicted with the condition. One is the neutral value and means that there is no difference between the groups compared; when the value is greater than one it means that there has been some difference between the two groups, whether it was caused by bias, chance, or an actual relationship between the exposure and outcome is yet to be seen. The P-value tells us whether the results of the study can be used. The P-value is the measure of how confident you are that your findings are correct. You can only trust your findings to be correct if the P-value is less than .05.
Odds Ratio - used in case-control study, [math]a \cdot d \over b \cdot c[/math]
Relative Risk - used in cohort study, [math]a/(a+b) \over c/(c+d)[/math]
Attack Rate - the rate that a group experienced an outcome or illness equal to the number sick divided by the total in that group. (There should be a high attack rate in those exposed and a low attack rate in those unexposed.)
- For the exposed: [math]\frac{a}{a+b}[/math]
- For the unexposed: [math]\frac{c}{c+d}[/math]
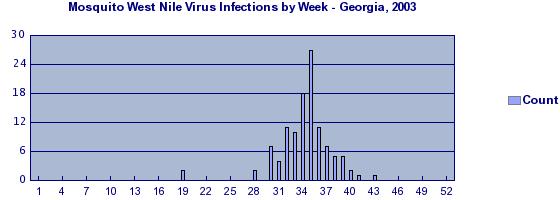
Using Epi-Curves
An epi-curve is a histogram that shows the course of an outbreak by plotting the number of cases of a condition according to the time of onset. Epi-Curves fall into three classifications:
Point source epidemics occur when people are exposed to the same exposure over a limited, well define period of time. The shape of the curve commonly rises rapidly and contains a definite peak, followed by a gradual decline.
Continuous common source epidemics occur when the exposure to the source is prolonged over an extended period of time and may occur over more than one incubation period. The down slope of the curve may be very sharp if the common source is removed or gradual if the outbreak is allowed to exhaust itself.
Propagated (progressive source) epidemics occur when a case of disease serves later as a source of infection for subsequent cases and those subsequent cases, in turn, serve as sources for later cases. The shape of this curve usually contains a series of successively larger peaks, reflective of the increasing number of cases caused by person-to-person contact, until the pool of those susceptible is exhausted or control measures are implemented. The distance between these peaks may be a rough indication of the incubation period of the disease. As the outbreak progresses, the peaks flatten out (think of the variance around a mean over multiple generations).
Validity of Study Results: Error and Bias
- Random error is the result of fluctuations around a true value because of the sample population. Random error can result from poorly worded questions or misunderstanding of questions. As the term implies, it is random, so it is impossible to correct. However, random error can be reduced; some ways include increasing the sample size and making measurements more precise, either by using a more accurate measurement device or by taking more trials. While these techniques would increase random error, they can also be expensive. Better measurement devices will cost more, and more trials and a larger sample size will mean more work.
- Precision is a measure of random error that is inversely related, so increasing random error decreases precision.
- Systematic error is any error other than random error. For example, systematic error can occur if the markings on your ruler are wider. This would make the numeric measurements less than what they actually are, making all data collected inaccurate. However, trends observed may still be preserved (shifting a line vertically preserves a line, as it is a rigid motion).
- Selection bias occurs when selection of participants for a study is affected by an unknown variable that is associated with the exposure and outcome being measured.
- Information bias occurs when bias is introduced through an error in measurement or observation
- An example of information bias is recall bias. When studied, some subjects may more easily recall specific habits related to a disease or condition than subjects not affected with the disease or condition.
- Confounding bias is bias resulting from mixing effects of several factors. Unlike selection and information bias, confounding bias deals with causation and not variations in study results.
Disease and Disease Transmission
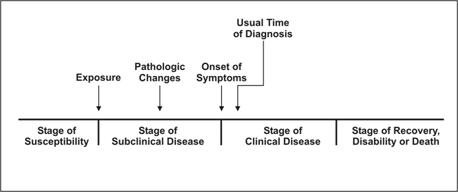
Natural History and Spectrum of Disease
The process begins with the appropriate exposure to or accumulation of factors sufficient for the disease process to begin in a susceptible host. For an infectious disease, the exposure is a microorganism. For cancer, the exposure may be a factor that initiates the process, such as asbestos fibers or components in tobacco smoke (for lung cancer), or one that promotes the process, such as estrogen (for endometrial cancer).
After the disease process has been triggered, pathological changes then occur without the individual being aware of them. This stage of subclinical disease, extending from the time of exposure to onset of disease symptoms, is usually called the incubation period for infectious diseases, and the latency period for chronic diseases. During this stage, disease is said to be asymptomatic (no symptoms) or inapparent. This period may be as brief as seconds for hypersensitivity and toxic reactions to as long as decades for certain chronic diseases. Even for a single disease, the characteristic incubation period has a range. For example, the typical incubation period for hepatitis A is as long as 7 weeks. The latency period for leukemia to become evident among survivors of the atomic bomb blast in Hiroshima ranged from 2 to 12 years, peaking at 6–7 years.
The onset of symptoms marks the transition from subclinical to clinical disease. Most diagnoses are made during the stage of clinical disease. In some people, however, the disease process may never progress to clinically apparent illness. In others, the disease process may result in illness that ranges from mild to severe or fatal. This range is called the spectrum of disease. Ultimately, the disease process ends either in recovery, disability or death.
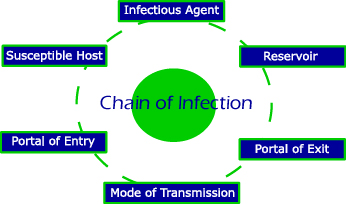
Chain of Infection
Agent leaves reservoir through portal of exit, and is conveyed by some mode of transmission, and enters the appropriate portal of entry to infect a susceptible host.
Agent - A microbial organism with the ability to cause disease.
Reservoir - A place where agents can thrive and reproduce.
Portal of Exit - A place of exit providing a way for an agent to leave the reservoir; the route a pathogen takes out of an infected host. Portals of exit tend to be fairly well defined. What serve as portals of exit are often not terribly surprising, at least, once something is known of how and where a pathogen replicates and enters new hosts. Respiratory infections tend to utilize the mouth and nose as portals of exit. Gastrointestinal diseases tend to exit in feces or saliva, depending on the site of replication. Sexually transmitted diseases tend to have portals of exit at the urethra or genital region. Blood-bourne diseases tend to exit via arthropods, needles, bleeding, or hyperdermic syringes. A more general portal of exit occurs when an infected animal is butchered or an infected person undergoes surgery. The three most common portals of exit are the skin, gastrointestinal tract, and respiratory tract.
Mode of Transmission - Method of transfer by which the organism moves or is carried from one place to another; the transfer of disease-causing microrganisms from one environment to another, particularly from an external environment to a susceptible individual. There are three general categories of transmission: contact, vehicle, and vector.
Portal of Entry - An opening allowing the microorganism to enter the host; the route a pathogen takes to enter a host. Just as with the portals of exit, many pathogens have preferred portals of entry. Many pathogens are not able to cause disease if their usual portal of entry is artificially bypassed. The most common portal of entry is the mucous membrane of the respiratory tract.
Susceptible Host - A person who cannot resist a microorganism invading the body, multiplying, and resulting in infection.
Chain of Infection: Diagram and Explanation
Characteristics of Agents
- Infectivity - capacity to cause infection in a susceptible host
- Pathogenicity - capacity to cause disease in a host
- Virulence - severity of disease that the agent causes to host
Modes of Disease Transmission
Contact Transmission - sub-categories include direct (person-to-person), indirect (fomite), or droplet.
- Direct Contact - occurs through touching, kissing, dancing, etc . To prevent direct contact transmission, wear gloves and masks, etc.
- Indirect Contact - occurs from a reservoir via inanimate objects called fomites. Fomites are basically almost anything an infected individual or reservoir can touch, upon which can be left a residue of contagious pathogen. Exceptions include the various inanimates ferred to as vehicles: food, air, and liquids. Typically, it is more difficult to avoid indirect contact transmission than it is to avoid direct contact transmission. A certain degree of organismal durability may be necessary to survive passage on a fomite. The best way to prevent indirect contact transmission is by avoiding contact with fomites, avoiding contact of hands with mucous membranes, especially when handling or potentially handling fomites, the use of barriers when handling fomites, and disinfecting fomites before handling.
- Droplet Transmission - consequence of being coughed, sneezed, or spit on. To be considered droplet transmission, mucous droplets must still be traveling with the velocity imparted on it leaving the mouth. As a rule of thumb, this is up to one meter after exiting the mouth. Any further and this is considered airborne transmission. Given interaction within one meter of people is certainly more difficult to avoid droplet transmission than it is to avoid either direct or indirect transmission. Not surprisingly, it is especially respiratory diseases that are transmitted by droplets.
Vehicle Transmission - transmission via a medium such as food, air, and liquid, which are all routinely taken into the body, and thus serve as vehicles into the body.
- Airborne Transmission - occurs via droplets (typically mucous droplets) where droplets are liquids that remain airborne whether as aerosols (very small droplets) or associated with dust particles. An example is within airliners where economizing measures reduces the turnover of cabin air and consequently increases air recycling. Organisms which can find their way into the air and remain viable thus have repeated opportunities to infect passengers. It requires greater organismal durability that droplet transmission simply because of the length of time the microorganism is exposed to the air, before infecting a new host, is longer. Increased durability is to the effects of desiccation, exposure to sunlight, etc. This is why breathing does not typically result in the acquisition of disease.
- Food-borne Transmission - any number of pathogens are found in food and not killed during processing may be transmitted via food product. Salmonella especially tends to be part of the normal flora of chickens and consequently associated with chicken products.
- Water-borne Transmission - fecal contaminated water. Generally, this is via sewage contaminated water supplies. It is especially gastrointestinal pathogens that are present in feces and therefore which rely on this type of transmission.
Vector Transmission - no entry.
- Portals of Entry to the Nervous System - the brain is typically fairly resistant to bacterial infection. There are four common portals of entry to the nervous system. For an organism to take advantage of these routes, they must display increasingly specialized adaptations as read from first to last: parenteral, via the blood, via the lymphatic systems, and up the peripheral nerve axons. Ordering of blood and lymphatic system was arbitrary and not intended to imply that one serves as a significantly more difficult portal to take advantage of than the other.
The scheme used by the American Public Health Association and CDC (Principles of Epi, 3rd edition) is a bit different. The 2 main categories are Direct and Indirect Transmission (not Contact). Direct Transmission includes Direct Contact and Droplet Spread. Examples of direct contact includes things like kissing, biting, and contact with soil containing infectious agents that penetrate the skin or enter wounds. Droplet spread is essentially an "in your face sneeze or cough". The idea is up close and immediate.
Indirect Transmission includes Airborne, Vehicles and Vectors. Airborne transmission involves dust or droplet nuclei (the latter are essentially little (<5 micron) particles that remain suspended in the air. Time and distance are both greater than for droplet spread (distance >6-8 ft). Vehicles include things like food, water, or fomites. Vehicles may passively carry pathogens or may promote growth or toxin production. Vectors are arthropods (e.g. mosquitoes, flies, lice, ticks) that spread infectious agents. If the agent multiplies or undergoes a change in life stage (as with malaria) within the vector, the vector is said to be a Biologic Vector. If the agent is simply carried from one place to another (think of a fly landing on feces and then a bowl of potato salad) it is a Mechanical Vector. Generally vector-borne diseases are thought of only in the context of biologic vectors. Rabies from a dog bite would be direct contact, not a vector. Note that while terms like food-borne, waterborne and zoonotic are not really included in this system - they are still valid.
Disease Prevention
For prevention strategies relating to the yearly topics, please see Disease Detectives#Yearly Topics.
- Primary prevention - early intervention to avoid initial exposure to agent of disease preventing the process from starting
- Secondary prevention - during the latent stage (when the disease has just begun), process of screening and instituting treatment may prevent progression to symptomatic disease
- Tertiary prevention - during the symptomatic stage (when the patient shows symptoms), intervention may arrest, slow, or reverse the progression of disease
- Quaternary prevention - set of health activities to mitigate or avoid consequences of unnecessary/excessive intervention of the health system. Social credit that legitimizes medical intervention may be damaged if doctors don't prevent unnecessary medical activity and its consequences.
In Disease Detectives scenarios, event supervisors will often ask you to brainstorm disease prevention methods. Even if you know very little about the disease, you can brainstorm ideas from the chain of infection for the disease. For example, if the chain of infection describes that a disease is comes in contact with humans through sand at the beach and enters the body through any openings (mouth, nose, etc.), a prevention method could be putting up signs at beaches reminding the public to wash their hands before consuming any food.
Immunity
- Active Immunity- occurs when the person is exposed to a live pathogen, develops the disease, and becomes immune as a result of the primary immune response
- Passive Immunity-short-term immunization by the injection of antibodies, such as gamma globulin, that are not produced by the recipient's cells. Naturally acquired passive immunity occurs during pregnancy, in which certain antibodies are passed from the maternal into the fetal bloodstream.
- Herd Immunity- protecting a whole community from disease by immunizing a critical mass of its populace. Vaccination protects more than just the vaccinated person. By breaking the chain of an infection’s transmission, vaccination can also protect people who haven’t been immunized. But to work, this protection requires that a certain percentage of people in a community be vaccinated.
Yearly Topics
Bear in mind that Disease Detectives no longer focuses on one topic; rather all topics are used in tests!
Foodborne Illness
Here are lists of foodborne illnesses, and other important information regarding foodborne illnesses: List You should know that this year, specific diseases are not included in tests and competitions!
FAT TOM
Is a device to describe the six favorable conditions required for the growth of foodborne pathogens. It is an acronym for food, acidity, time, temperature, oxygen, and moisture.
| F | Food | There are sufficient nutrients available that promote the growth of microorganisms. Protein-rich foods, such as meat, milk, eggs, and fish are the most susceptible. |
|---|---|---|
| A | Acidity | Foodborne pathogens require a slightly acidic pH level of 4.6-7.5, while they thrive in conditions with a pH of 6.6-7.5. The United States Food and Drug Administration's (FDA) regulations for acid/acidified foods require that the food is to be brought to pH 4.5 or below. |
| T | Time | Food should be removed from "the danger zone" (see below) within two-four hours, either by cooling or heating. While most guidelines state two hours, a few indicate four hours is still safe. |
| T | Temperature | Food-borne pathogens grow best in temperatures between 41 to 135 °F (5 to 57 °C), a range referred to as the temperature danger zone (TDZ). They thrive in temperatures that are between 70 to 104 °F (21 to 40 °C). |
| O | Oxygen | Almost all foodborne pathogens are aerobic, that is requiring oxygen to grow. Some pathogens, such as Clostridium botulinum, the source of botulism, are anaerobic. |
| M | Moisture | Water is essential for the growth of foodborne pathogens, water activity (aw) is a measure of the water available for use and is measured on a scale of 0 to 1.0. Foodborne pathogens grow best in foods that have aw between 0.95 and 1.0. FDA regulations for canned foods require aw of 0.85 or below. |
Prevention
For Food Borne Illnesses, prevention tactics include:
- Cook meat, poultry, and eggs thoroughly.
- Don't cross-contaminate one food with another.
- Chill and refrigerate leftovers promptly.
- Clean and wash all produce.
- Report suspected foodborne illnesses to the local health department.
Environmental Quality
This topic is incomplete. |
Environmental quality typically deals with biological, chemical, and physical causes of illness. This can include air, water or noise pollution; smoking; natural disasters (flooding, drought, etc.); effects of toxins and pesticides, and more.
Population Growth
This topic is incomplete. |
Population growth follows factors that have come out of the growing world population, and what larger organizations have done to help. It also talks about relevant epidemics (like the flu) that have come out of population growth.
Statistics
This section is incomplete. |
For Division C, statistics is a crucial part of the event (even though the rules specify that it should be less than 10% of the test material). Understanding statistics can be the difference between a good disease detective and an excellent disease detective. However, many disease detectives only make an effort to know the formulas that compute certain statistical measures without delving into the deeper (highly interesting!) meaning of statistics.
Basics
This is a crash course on the fundamentals of statistics. This is not a replacement for reading (and understanding) the SOINC guide on statistics in this event or better yet, taking a class or reading a textbook on statistics.
Populations and Samples
The population is the entire set under study. For example, the length of dung beetles. Because it is impossible to measure the length of every single dung beetle on planet earth, statistics use sampling. They take a subset of the dung beetles called a sample and use measurements from the sample to make inferences about the population as a whole. A population parameter is a characteristic of a population; for example, suppose 84% of Philadelphians preferred chocolate ice cream over vanilla ice cream. A sample statistic is an attribute of a sample; for example, we randomly sampled 10 Philadelphians and found that 70% preferred chocolate ice cream over vanilla ice cream.
Distribution Characteristics
Distributions are characterized by center, shape, and spread.
Central Tendency
A central tendency is a "typical" or "middle" value for a distribution.
Mean - Average of all of the values. [math]A=\dfrac{a_{1}+a_{2}+a_{3}...}{n}[/math] Means should not be used if the population is very skewed, as means are easily affected by extreme values.
Median - The middle value that separates the data into two halves. Medians are not as affected by extreme values, e.g. the mean number of arms per person in the world is less than 2, but the median is exactly 2.
Mode - The most frequently occurring value in the data set. Modes are useful for describing "peaks" in a distribution.
Shape
Skewedness - Distributions that have a few extreme values on the higher side are skewed to the right. Distributions that have a few extreme values on the lower side are skewed to the left.
Peaks - If a distribution has no peaks, it is uniform. If it has one peak, it is unimodal. If it has two peaks, it is bimodal.
Normal distributions - A set of data that is unimodal, symmetrical, and continues off to infinity on both tails. Also known as a Gaussian distribution. In the normal distribution, the mean, median, and mode are all the same. Technically, the normal distribution is continuous and infinite but can be approximated with discrete values.
Variability
Variability, scatter, and spread all have the same meaning: the extent to which a set of data is dispersed.
Range - The difference between the largest and smallest values in a set. It is not very useful except to get a sense of the possible spread of a distribution.
Interquartile Range (IQR) - The difference between the 75th (third quartile, or [math]Q_{3}[/math]) and 25th (first quartile or [math]Q_{1}[/math]) percentiles of a data set. To find [math]Q_{1}[/math] and [math]Q_{3}[/math], find the median of the data set, then divide the data set into two new sets, one with the data from the median up to the maximum and the other with the data from the median down to the minimum. The median values of the two new sets are [math]Q_{1}[/math] and [math]Q_{3}[/math]. The IQR is used with the median and is the most robust measure of variability, i.e. outliers do not affect the IQR as much. [math]IQR=Q_{3}-Q_{1}[/math]
Variance - Average of the squared differences from the mean. The variance gives a very vague sense of how far apart the values in a data set are compared to the mean. [math]Var(x)=\dfrac{\sum(x-\bar{x})^2}{n-1}[/math]
Standard Deviation (SD) - The square root of the variance. Quantifies the spread in a data set in the same units as the original data. Standard deviation is, in a sense, the average distance away from the mean. A low SD indicates that the data tends to be close to the mean and a high SD indicates the data is far away from the mean. SD and variance are used with the mean. Unlike IQR, SD is not resistant to outliers.
[math]SD(x)=s=\sqrt{\dfrac{\sum(x-\bar{x})^2}{n-1}}[/math]
68-95-99.7 Rule - This rule states that 68% of the values in a normally distributed data fall within 1 SD of the mean, 95% fall within 2 SD of the mean, and 99.7% fall within 3 SD of the mean.
Example: Let a data set consist of integers 1 through 10, which sum to 55. The median and mean are 5.5.
To find the IQR, we can divide the data into two sets, one from 1 through 5 and the other from 6 through 10 inclusive. We find the median for each of these sets (3 and 8) and then subtract them. Thus, the IQR is 5.
To find the SD, we need to calculate the difference of each data value from the mean. Then we square the differences, add them, divide it by the sample size - 1 [math](n=10, n-1=9)[/math] and square root the result.
[math]SD(x)=\sqrt{\dfrac{(1-5.5)^2+(2-5.5)^2+...+(10-5.5)^2}{9}}=2.87[/math]
Note that this population is uniform (each possibility has the same frequency of occurring), so the 68-95-99.7 rule for normal distributions does not apply. If it did apply, 68% of the data would fall in between the interval [math](5.5-2.87, 5.5+2.87)=(2.63, 8.37)[/math].
Standard Error of the Mean (SEM) - The SEM measures the variability of the mean of different samples around the population mean.
[math]SE_{\bar{x}}=\dfrac{s}{\sqrt{n}}[/math]
Therefore, as a general rule, the SEM decreases as sample size increases.
Correlation
When two variables are revealed to have a relationship using statistical measures, the variables have a correlation. This correlation can be positive, negative, or zero. Without doing an experiment or trial, it is impossible to conclude that one variable causes another variable to act in some way. There is always the possibility of a third lurking or confounding variable that the original data does not account for. In this case, wording is extremely important. Correlation [math]\neq[/math] causation.
The correlation coefficient [math]r[/math] is a measure of the scatter around a linear relationship. It does NOT apply when a relationship is non-linear. Because the correlation coefficient is difficult to calculate by hand, exam writers will typically give the value and ask for the interpretation of the [math]r[/math] value. The correlation coefficient is always [math]-1<r<1[/math] and a value of 1 indicates a perfectly positively linear relationship. Conversely, a value of 0 indicates no relationship. Typically, [math]0.9<|r|<1[/math] is termed strong.
Standardization
The standard score or z score rescales the standard deviation of a normally distributed data set to 1 and mean to 0. Thus, we can model all normally distributed data using a single normal distribution with mean 0 and SD 1.
[math]z=\dfrac{x-\mu}{\sigma}=\dfrac{x-\bar{x}}{s}[/math]
The first formula is for a population while the second is for a sample. [math]\sigma[/math] represents the population standard deviation while [math]\mu[/math] represents the population mean.
Infant Mortality Rate
The infant mortality rate is the ratio of deaths to births.
Rates in epidemiology are often expressed as a per-1000 or per-1 million, so if the infant mortality rate were 0.05, we could write that as 50 deaths per 1000 births.
Inference
Statistical inference is the process of inferring something about a population given a sample.
Confidence Intervals
Confidence intervals are used to estimate population attributes given statistics from a sample. However, confidence intervals do not take into account confounding or biases. The confidence level determines how wide the interval is. A common confidence level is 95%: "I am 95% certain that the interval captures the true population proportion/mean. This means that if the process used to obtain the interval were repeated many, many times, the interval generated would capture the true population proportion/mean 95% of the time."
Confidence Intervals for Proportions - Used to define a range of values within which a proportion may lie.
[math]\hat{p}\pm z^{*}\sqrt{\frac{\hat{p}(1-\hat{p})}{n}}[/math]
A z table contains common values for z-star.
Confidence Intervals of Means - Used to define a range of values within which a mean may lie.
[math]\bar{x}\pm t^{*}\frac{s}{\sqrt{n}}[/math]
A t table contains common values for t-star. Note that you need the number of degrees of freedom (df) to find the t-star. Generally, [math]df=n-1[/math].
Inference Tests
In an inference test, we use statistical inference to determine if a statement is likely or unlikely. We first create a null hypothesis ("the default"). For example, suppose that you were investigating whether drinking the punch at the party is associated with developing salmonellosis symptoms. The null hypothesis would be that eating cabbage is not associated with developing salmonellosis symptoms. The alternative hypothesis would be that eating cabbage is associated with developing salmonellosis symptoms. You would then look at your sample (people who were at the party and did/did not drink the punch and did/did not develop salmonellosis symptoms) and ask, How likely is it that this result occurred by chance, i.e. if the null hypothesis were true? This probability is called the p-value. Statisticians generally use a threshold of 0.05. If the p-value is below 0.05, the result is significant, and you reject the null hypothesis. Otherwise, you fail to reject the null hypothesis.
Error
A Type I error occurs if you reject [math]H_o[/math] (the null hypothesis) when [math]H_o[/math] is true. The probability of a Type I error is [math]\alpha[/math], the significance level.
A Type II error occurs if you fail to reject [math]H_o[/math] when [math]H_o[/math] is false ([math]H_a[/math] is true). The probability of a Type II error is represented by the letter [math]\beta[/math].
The power of the test is the probability that the null hypothesis is rejected if [math]H_o[/math] is false. The power of the test is equal to [math]1-\beta[/math].
Advanced
Sensitivity and Specificity
Sensitivity and specificity are ways to calculate the chance of having a specific disease given you do or do not have a disease.
| Has disease | Has no disease | |
|---|---|---|
| People who test positive | a | b |
| People who test negative | c | d |
Sensitivity is the chance of testing positive if you do have the disease. The equation to use for sensitivity is: [math]a \over a+c[/math]
Specificity is the chance of testing negative if you do not have the disease. The equation to use for specificity is: [math]d \over d+b[/math]
Chi Square
A chi-square is a statistical measure used to determine the difference between an expected value and an observed value. In epidemiology, it can be used to compare information from different groups (i.e. age) to a local or national average. [math]\chi^2=\sum\frac{(O−E)^2}{E}[/math]
Z-Test
Used to compare two means when the population variances are known and the sample size is greater than 30
T-Test
Used to compare two means when sample size is greater than 30
Paired T-Test
Used to compare multiple sets of data
Fischer's Exact Test
Fischer's test searches for non-random associations between two categorical variables.
McNemar's Test
The McNemar Test is similar to a Chi-Square, except that it uses matched paired data.
Maentel Haenszel Test
The Cochran-Maentel-Haenszel Test aims to find the association between variables while controlling for confounding.
ANOVA
The analysis of variance test, or ANOVA, is a statistical measure used to compare two or more means.